What are Safety metrics? Identifying the optimal Safety metrics can be challenging, especially when everyday tasks consume your time. To help you, we've assembled a list of examples to ignite your creativity.
Copy these examples into your preferred app, or you can also use Tability to keep yourself accountable.
Find Safety metrics with AI While we have some examples available, it's likely that you'll have specific scenarios that aren't covered here. You can use our free AI metrics generator below to generate your own strategies.
Examples of Safety metrics and KPIs 1. Incident Rate Measures the number of safety incidents per number of hours worked, indicating overall workplace safety.
What good looks like for this metric: 3.0 incidents per 100 employees annually
Ideas to improve this metric Conduct regular safety audits Enhance employee safety training programs Implement stricter safety protocols Improve incident reporting systems Involve employees in safety planning 2. Training Completion Rate Percentage of employees who have completed required safety training within a set time period.
What good looks like for this metric: 95% completion rate
Ideas to improve this metric Automate training reminders Provide flexible training schedules Incorporate online training modules Track progress with a learning management system Reward timely completion with incentives 3. Audit Finding Closure Rate Percentage of identified compliances or safety issues that have been addressed within a designated time frame.
What good looks like for this metric: 100% closure within 30 days
Ideas to improve this metric Assign responsibilities for issue resolution Set clear deadlines for issue closure Monitor progress with regular check-ins Establish a robust feedback mechanism Use software tools to track progress 4. Employee Safety Observation Frequency Frequency of safety observations made by employees, indicating proactive safety engagement.
What good looks like for this metric: 2 observations per employee per month
Ideas to improve this metric Encourage a culture of safety communication Provide easy tools for reporting observations Recognise employees for contributing observations Conduct regular safety awareness campaigns Offer training on identifying potential hazards 5. Cost of Compliance Management Total cost incurred in ensuring compliance with safety standards, as a percentage of overall operational cost.
What good looks like for this metric: 3-5% of total operational cost
Ideas to improve this metric Identify cost-effective compliance tools Negotiate better terms with compliance vendors Streamline compliance processes Automate repetitive compliance tasks Analyze cost-effectiveness of current strategies
← →
1. Infection Rate Reduction The measure of reduction in infection cases reported in the facility after renovations
What good looks like for this metric: A typical benchmark is a 20% reduction in infection rates
Ideas to improve this metric Conduct regular infection audits Ensure proper sanitisation of equipment Implement staff training on infection control Enhance air filtration systems Utilise antimicrobial surfaces 2. Patient Safety Incident Count Number of safety-related incidents reported per 1,000 patient days
What good looks like for this metric: Aim for fewer than 10 incidents per 1,000 patient days
Ideas to improve this metric Standardise safety protocols Improve staff communication channels Introduce safety drills and training Enhance surveillance systems Regularly update safety guidelines 3. Workflow Efficiency Percentage Percentage of processes completed within the expected time frame
What good looks like for this metric: Achieving at least 85% on-time process completion
Ideas to improve this metric Optimise staffing schedules Implement workflow management software Regularly review and adjust processes Conduct time management training Utilise feedback to streamline operations 4. Patient Satisfaction Scores Patients' average satisfaction rating post-renovation
What good looks like for this metric: A target of at least 90% satisfaction
Ideas to improve this metric Enhance waiting area conditions Provide clear communication about changes Solicit frequent patient feedback Ensure staff are attentive and responsive Provide patient education on safety improvements 5. Staff Compliance Rate with Protocols Percentage of staff compliance with updated infection control protocols
What good looks like for this metric: Aim for at least 95% compliance
Ideas to improve this metric Incentivise adherence to protocols Conduct regular staff assessments Provide ongoing training sessions Utilise visual reminders and aids Implement a peer review system
← →
1. Number of Parameters Differentiates model size options such as 1 billion (B), 3B, 7B, 14B parameters
What good looks like for this metric: 3B parameters is standard
Ideas to improve this metric Evaluate the scalability and resource constraints of the model Optimise parameter tuning Conduct comparative analysis for various model sizes Assess trade-offs between size and performance Leverage model size for specific tasks 2. Dataset Composition Percentage representation of data sources: web data, books, code, dialogue corpora, Indian regional languages, and multilingual content
What good looks like for this metric: Typical dataset: 60% web data, 15% books, 5% code, 10% dialogue, 5% Indian languages, 5% multilingual
Ideas to improve this metric Increase regional and language-specific content Ensure balanced dataset for diverse evaluation Perform periodic updates to dataset Utilise high-quality, curated sources Diversify datasets with varying domains 3. Perplexity on Validation Datasets Measures the predictability of the model on validation datasets
What good looks like for this metric: Perplexity range: 10-20
Ideas to improve this metric Enhance tokenization methods Refine sequence-to-sequence layers Adopt better pre-training techniques Implement data augmentation Leverage transfer learning from similar tasks 4. Inference Speed Tokens processed per second on CPU, GPU, and mobile devices
What good looks like for this metric: GPU: 10k tokens/sec, CPU: 1k tokens/sec, Mobile: 500 tokens/sec
Ideas to improve this metric Optimise algorithm efficiency Reduce model complexity Implement hardware-specific enhancements Utilise parallel processing Explore alternative deployment strategies 5. Edge-device Compatibility Evaluates the model's ability to function on edge devices with latency and response quality
What good looks like for this metric: Latency: <200 ms for response generation
Ideas to improve this metric Optimise for low-resource environments Develop compact model architectures Incorporate adaptive and scalable quality features Implement quantisation and compression techniques Perform real-world deployment tests
← →
1. Training Completion Rate The percentage of staff who have completed the training program on infectious diseases and PPE preparations.
What good looks like for this metric: 90% completion rate
Ideas to improve this metric Create a mandatory training schedule Send regular reminders to complete training Offer incentives for early completion Provide flexible training times Ensure easy access to training materials 2. Post-Training Assessment Scores The average score of staff on assessments conducted after training to evaluate understanding and retention of information.
What good looks like for this metric: 75% average score
Ideas to improve this metric Enhance the clarity of training materials Incorporate interactive learning methods Provide additional resources for self-study Offer review sessions or refresher courses Implement individualized feedback on assessments 3. PPE Usage Compliance The percentage of staff correctly using PPE as per guidelines during drills or assessments.
What good looks like for this metric: 95% compliance
Ideas to improve this metric Conduct regular PPE drills Provide clear PPE usage guidelines Supervise and guide during PPE drills Offer corrective training for non-compliance Use checklists for PPE usage 4. Feedback from Participants The qualitative and quantitative feedback collected from staff about the effectiveness of the training program.
What good looks like for this metric: 4 out of 5 average rating
Ideas to improve this metric Conduct anonymous surveys post-training Hold feedback sessions with experienced trainers Implement a feedback loop to improve training Encourage open communication for suggestions Act on feedback promptly to show responsiveness 5. Incident Reporting Rate The number of infectious disease incidents reported and managed correctly post-training compared to pre-training.
What good looks like for this metric: Decrease by 30% post-training
Ideas to improve this metric Improve ease of incident reporting procedures Encourage a culture of transparency and safety Highlight the importance of prompt reporting Facilitate regular training refresher sessions Analyse incident data to prevent future occurrences
← →
1. Food Quality Rating Assesses the quality of food served based on customer feedback and reviews
What good looks like for this metric: 4.5 out of 5 stars
Ideas to improve this metric Conduct regular taste tests Solicit customer feedback Ensure fresh ingredients Train staff on culinary skills Regularly review and update recipes 2. Recipe Consistency Score Measures the consistency of recipes across different chefs and shifts
What good looks like for this metric: 90% consistency rate
Ideas to improve this metric Provide detailed recipe guides Use standardised measurements Conduct chef training sessions Regularly audit kitchen practices Set up a feedback loop with chefs 3. Employee Training Hours Tracks the number of training hours completed by employees to ensure high food quality and service standards
What good looks like for this metric: 20 hours per employee per year
Ideas to improve this metric Schedule regular training sessions Incorporate online learning modules Offer cross-training opportunities Practice skill assessments Incentivise training completion 4. Food Cost Percentage Indicates the percentage of revenue spent on food costs
What good looks like for this metric: 28% to 35%
Ideas to improve this metric Negotiate better supplier deals Conduct inventory audits regularly Implement portion control measures Analyse menu profitability Minimise food waste 5. Food Safety Compliance Rate Measures compliance with food safety regulations and standards
What good looks like for this metric: 100% compliance
Ideas to improve this metric Conduct regular safety training Implement a HACCP plan Use food safety checklists Conduct routine kitchen inspections Maintain equipment cleanliness
← →
1. CLABSI Incidence Rate The number of central line-associated bloodstream infections per 1,000 central line days
What good looks like for this metric: Typical rates are below 1.0 per 1,000 line days
Ideas to improve this metric Ensure adherence to insertion and maintenance protocols Conduct routine infection control training for staff Implement a checklist for central line insertion Review and enhance hand hygiene adherence Utilise antimicrobial-impregnated catheters 2. Central Line Utilisation Ratio The proportion of patient days for which central lines are used
What good looks like for this metric: Aim for a ratio below 0.5
Ideas to improve this metric Assess necessity of central lines daily Opt for alternative access methods when possible Educate staff on risks of unnecessary central line usage Implement daily rounds to evaluate central line need Standardize criteria for central line removal 3. Hand Hygiene Compliance Rate The percentage of times hand hygiene is properly performed as per the protocol before and after handling central lines
What good looks like for this metric: Target compliance rate of ≥90%
Ideas to improve this metric Install hand hygiene stations near patient beds Use electronic monitoring systems for hand hygiene Conduct regular compliance audits Provide feedback to staff on hand hygiene performance Introduce incentives for high compliance rates 4. Catheter Duration Average duration (in days) central lines are kept in place
What good looks like for this metric: Strive for minimal duration necessary for patient care
Ideas to improve this metric Review catheter need daily with a multidisciplinary team Set standard guidelines for acceptable catheter duration Promote patient involvement in daily catheter necessity evaluation Train staff to identify early signs of infection Utilize IT solutions to track catheter data and prompt removal 5. Staff Training Hours on CLABSI Prevention The total number of training hours completed by staff on preventing CLABSI annually
What good looks like for this metric: Minimum of 10 hours per staff member annually
Ideas to improve this metric Schedule regular training sessions throughout the year Incorporate e-learning modules for flexible access Engage staff with simulation-based learning Utilise external experts for specialized training Evaluate training effectiveness with pre- and post-tests
← →
1. Adherence to Design Specifications Measures the extent to which road maintenance work aligns with predefined design specifications
What good looks like for this metric: 90% or above compliance rate
Ideas to improve this metric Conduct regular design specifications training Implement stricter quality control checks Utilise advanced design software tools Ensure clear communication of specifications Collaborate with design experts 2. Quality of Materials Used Assesses the quality of materials used against standard requirements
What good looks like for this metric: 95% or above material quality rating
Ideas to improve this metric Use reputable material suppliers Test materials prior to use Adopt usage of high-grade materials Train staff on material standards Set up a material review board 3. Time to Completion vs Planned Schedule Compares the actual completion time of road maintenance projects to the planned schedule
What good looks like for this metric: Projects completed on or before schedule 80% of the time
Ideas to improve this metric Enhance project planning processes Allocate resources more efficiently Regularly review project timelines Minimise project scope changes Improve coordination among teams 4. Cost Adherence to Budget Tracks the extent to which actual expenditures align with budgeted costs for maintenance projects
What good looks like for this metric: Costs remain within 5% of budget
Ideas to improve this metric Conduct thorough cost estimates Implement stringent cost control measures Regular budget reviews and adjustments Negotiate better rates with suppliers Automate budget tracking and reporting 5. Safety Incident Rate Monitors the frequency of safety incidents occurring during maintenance work
What good looks like for this metric: Less than 1 incident per 1000 work hours
Ideas to improve this metric Strengthen safety training programs Introduce more comprehensive safety protocols Increase frequency of safety audits Encourage reporting of near misses Improve safety equipment and gear
← →
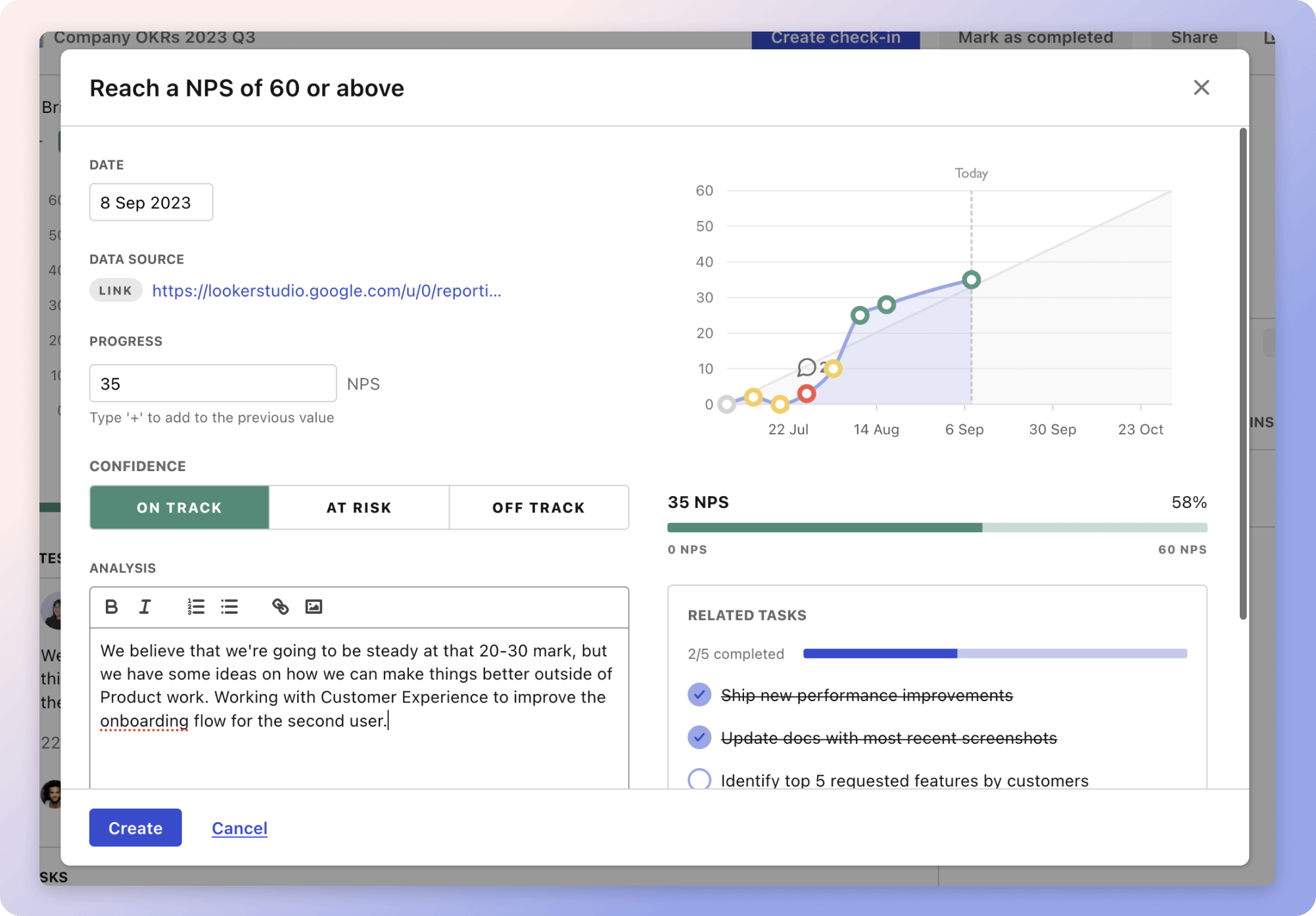
Tracking your Safety metrics Having a plan is one thing, sticking to it is another.
Don't fall into the set-and-forget trap. It is important to adopt a weekly check-in process to keep your strategy agile – otherwise this is nothing more than a reporting exercise.
A tool like Tability can also help you by combining AI and goal-setting to keep you on track.
More metrics recently published We have more examples to help you below.
Planning resources OKRs are a great way to translate strategies into measurable goals. Here are a list of resources to help you adopt the OKR framework:
 Tability's check-ins will save you hours and increase transparency
Tability's check-ins will save you hours and increase transparencyThe best metrics for Social Media Strategy Development
The best metrics for Communication and Marketing Officer
The best metrics for Class Preparation and Time Management
The best metrics for Operational Plan Execution
The best metrics for Manage a Southern Soul Food Restaurant
The best metrics for Evaluating Unit Revenue Performance